64 year old who is unable to talk since 1 day
Varsha bandaru
Roll no 07
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
CASE:
CHIEF COMPLAINTS:
Patient came to casuality with chief complaints of
- unable to talk since 1 day
- hiccups since 7 days
- bowel and bladder incontinence, loss of appetite since 3 days
- loose stools 5 days back relieved on medication
- fever 4 days back
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 7 days back , he then developed hiccups , loss of speech
- 5 days back he developed diarrhoea 5 episodes/ day , for one day which was relieved on medication
-loss of appetite since 3 days , since one day he is unable to talk
- No H/O SOB , cough , palpitations
- No H/O loss of consciousness , giddiness , involuntary passage of urine and stools .
PAST HISTORY:
h/o panic attack one month back secondary to family issues
- K/C/O DM2 since 2 yrs , on medication ,
-tab Metformin OD , tab Glimiperide OD
- Not a K/C/O HTN, TB, Asthma, epilepsy, CAD, CVD
PERSONAL HISTORY:
Appetite - lost
Diet - Mixed
Sleep - adequate
Bowel and bladder movements - incontinence
Addictions: Occasional alcoholic ( during functions ) , tobacco chewing occasionally
Allergies : No allergies
FAMILY HISTORY: Not significant
GENERAL EXAMINATION:
Patient is conscious ,incoherent , uncooperative
Moderately Built and Moderately Nourished .
Pallor : present
Icterus : absent
Cyanosis: absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
His vitals :-
Temp: Afebrile
BP : 100 / 50 mmHg
PR : 120 bpm
RR : 16 cpm
SPO2 : 98 % at RA
GRBS : 193 mg/dl
SYSTEMIC EXAMINATION :
CNS examination :-
State of consciousness : conscious
Speech : incoherent
Kernigs sign :- positive
Sensory system :-
Pain - Normal
Touch- fine touch - normal
crude touch - normal
Temp - normal
Vibration - normal
Joint position - normal
Cranial nerves : intact
CNS :-
Right. Left
Tone :- UL N. N
LL. N. N
Power :- UL. 5/5. 5/5
LL 5/5 5/5
Reflexes :-
Biceps + +
Tricep s + +
Supinator + +
Knee + +
Ankle. ++
Flexor. Plantar. Plantar
Finger nose in coordination - no
Heel knee in coordination - no
CVS : S1 S2 + ,no murmurs ,no thrills
Respiratory System : decreased air entry on left side . Diffuse crepts on left side. Position of trachea - central.
Per abdominal examination:-
Soft , non tender , no signs of organomegaly
Investigations:-
ECG
CHEST XRAY PA VIEW:
USG abdomen :
MRI BRAIN :
Hemogram
RBS:
LFT :
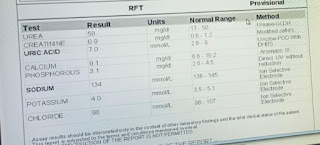
Serum creatinine :
Serum electrolytes :
provisional diagnosis:-
CVA: cerebro vascular accident .
Management:-
1) IVF 0.9 %NS IV @ 50 ml / hr
2) Inj , 1 amp Optineuron in 500 ml NS IV /OD
3) tab Ecosprin AV 75/10 RT / OD / HS
4) GRBS monitoring 6 th hrly
5) Inj Thiamine 200 mg IV/BD in 100 ml NS














Comments
Post a Comment