62 year old with pedal edema and facial puffiness since 3 days
Varsha Bandaru
Roll no 07
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
CASE :
HISTORY Of PRESENT ILLENESS :
Patient was apparently asymptomatic 30 years back then she developed fever and cough for which visited a local hospital where she was diagnosed with sputum positive TBand used ATT for 6 months and she recovered from then she was apparently asymptomatic 20 days back then she developed of fever for 2 days insidious onset , gradually progressive , low grade fever , intermittent in nature , relieved on medication , not associated with chills and rigors and weight loss.
2 days later H/0body pains aggregavated while working in her farm for which she used analgesics .
2 days later
she developed pedal edema and facial puffiness
Pedal edema - pitting type below the knees
For which visited a local hospital in miryalaguda where she was told to have a kidney problem later she visited our hospital for the same problem where she was evaluated and was initiated on haemodialysis
No history of decreased urine output, No history of haematuria
No H/o burning , NO H/O shortness of breath , cough , palpations.
No H/O loss of consciousness , giddiness, involuntary passage of urine and stools .
PAST HISTORY:
K/C/O of TB 30 years back used ATT for 6 months
Not a K/C/O HTN , ,Asthma , Epilepsy , CAD , CVD
PERSONAL HISTORY:
Appetite : lost
Diet : mixed
Sleep : Adequate
Bowel and bladder movements: Regular
Addictions : Toddy ( occasionally)
Allergies : No allergies
Family history: Not significant
GENERAL EXAMINATION:
Patient is conscious , cohorent , cooperative , moderately built and moderately nourished .
Pallor : present
Icterus : absent
Cyanosis : absent
Clubbing : absent
Lymphadenopathy: absent
Edema : present
Temperature : afrebrile
Pulse rate : 102bpm
RR:
Blood pressure:
Spo2:
Systemic examination :
Cardiovascular system:
Inspection
Apperas normal in shape
Apex beat not visible
No scars , sinuses , dilated veins
Palpation:
All inspectory findings are confirmed
Trachea central in position
Apex beat : 5 th intercostal space .5cm from medial to midclavicular line
Auscultation:
S1 and S2 heard
Respiratory system :
Trachea centrally located
Shape of chest : bilaterally symmetrical and elliptical
Auscultation: NVBS heard in infraaxillary, infrascapular and interscapular regions
Central nervous system :
No abnormal deficits
Per abdomen : soft and non tender ; no organomegaly
Liver not palpable
Spleen : not palpable
Bowel sounds heard
Provisional diagnosis ? Renal failure , AKI
Investigations :
E/ O Multiple cysts noted bilateral kidneys largest
26*21mm in left side
29*23 mm in right side
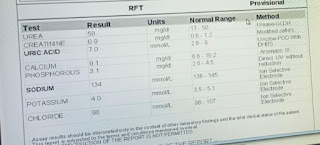
Renal function tests and electrolytes:
ECG :
Final diagnosis : Polycystic kidney disease
? AKI on CKD
History of pulmonary TB 30 years back
Treatment:
Tab lasix 40 mg
Tab orofer
Two session dialysis is done














Comments
Post a Comment